health3d.ai
“It is important to know what sort of person has disease then to know what sort of disease a person has”
We look at all facets of an individual to really define him or her
- Medical (medical history, family history, biological)
- Social (including environmental)
- Behavioral
Risk Score
Real Time
Real Solutions
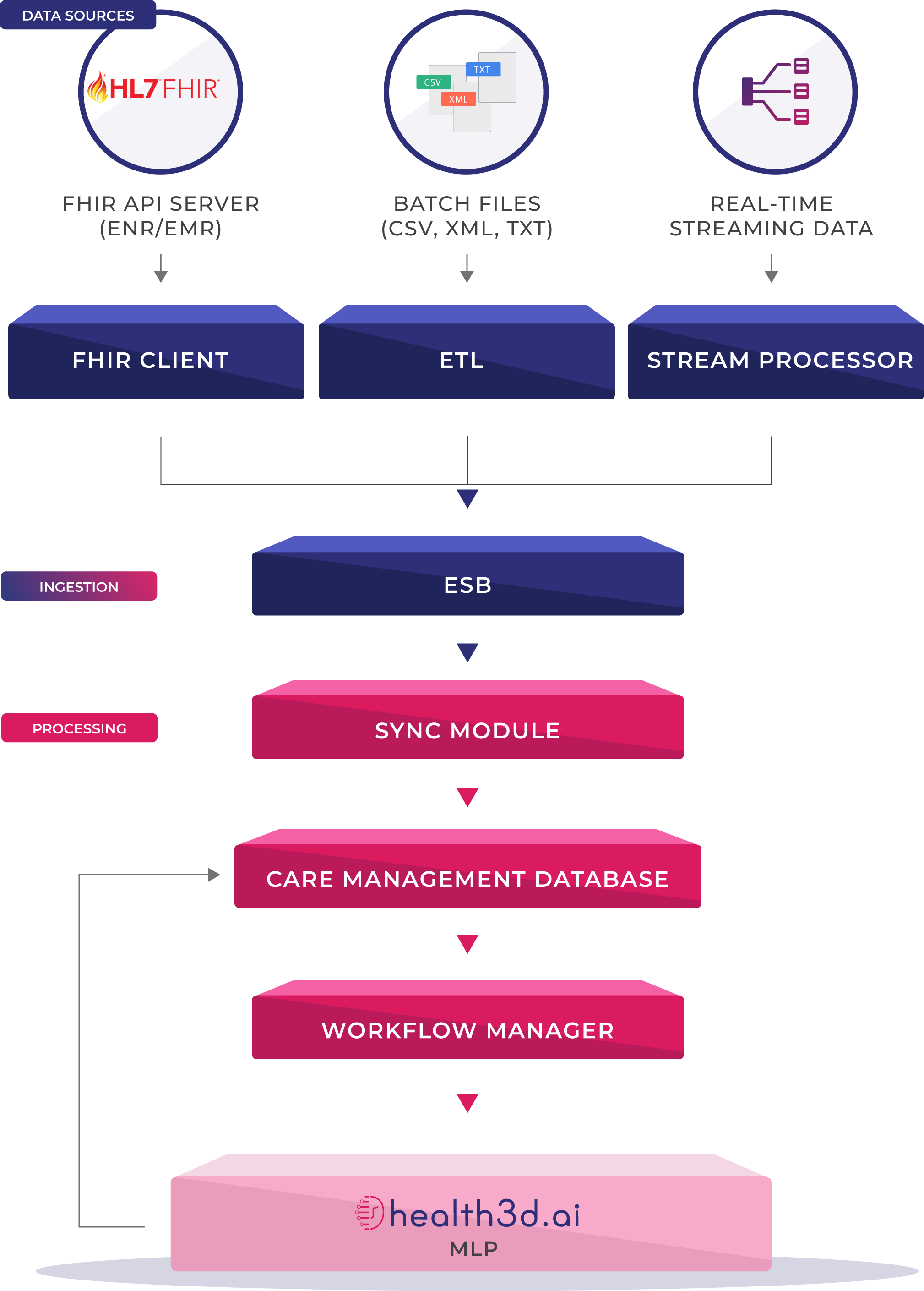
Data Processing & ETL
We designed health3D.ai to support Streaming ETL (aka real time ETL) to support real-time integration which helps in keeping longitudinal patient record and other critical patient data and transactions up to date and enhances the accuracy of analytics driven from the data warehouse.
Most modern EMR platforms (Cerner, EPIC, OpenMRS etc) support FHIR/HL7 based API out of the box.
While health3D.ai can do traditional file exchange and ETL/ELT based data loading, it has support for FHIR based APIs and traditional ETL based on HL7/FHIR format.
- Medical Claims
- Pharmacy Claims
- Lab
- Social Determinants
- Assessments
- Genomic
- Sensors
- EMR/EHR case notes
- Social Media
- Allergies
- Vitals
- Fitness Devices
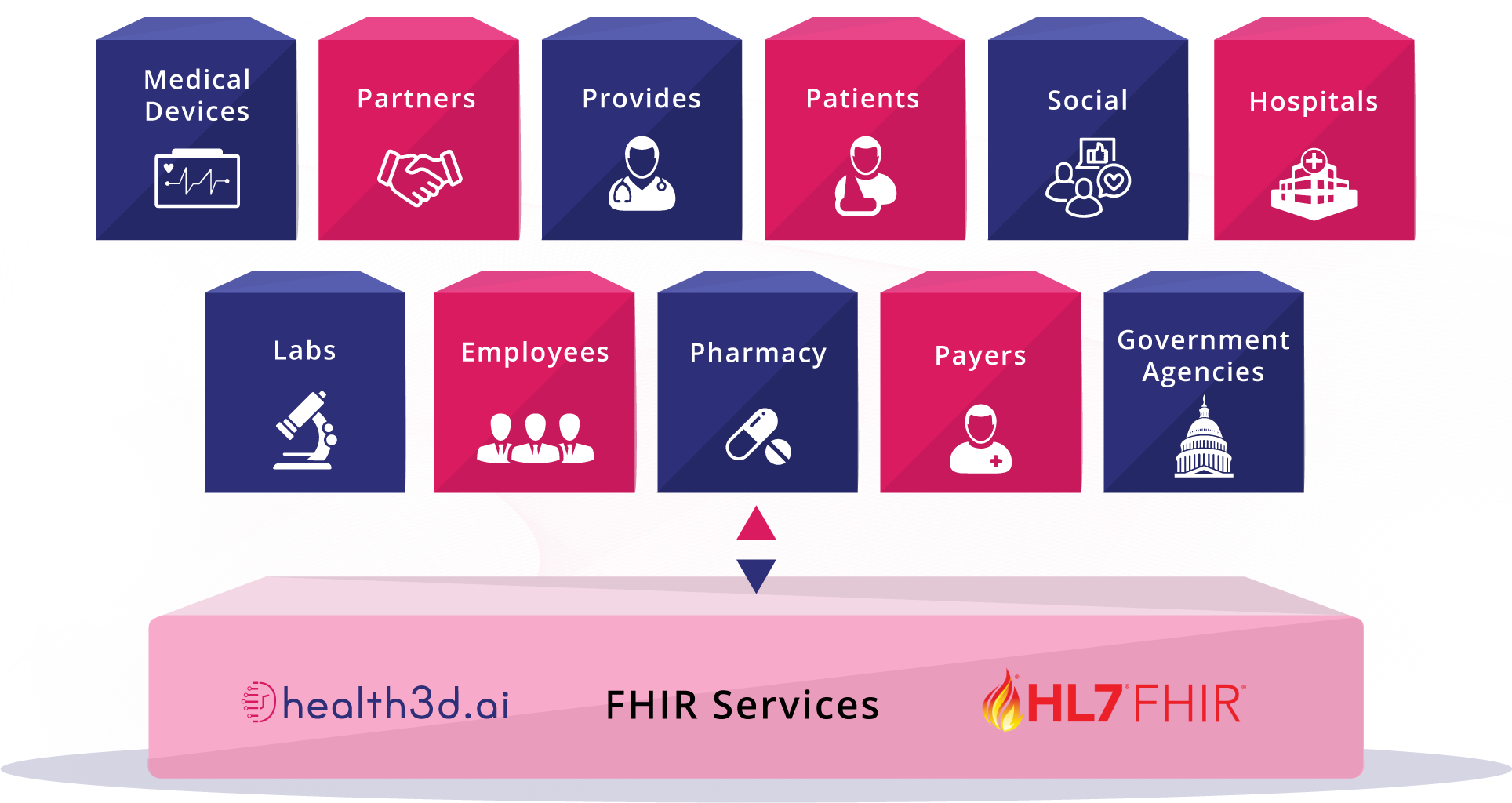
FHIR Interoperability
By Jan. 1, 2021, the CMS rule requires Qualified Health Plans in federally facilitated exchanges to deploy application programming interfaces (APIs) that can share patients’ data with any third-party app selected by a patient.
Medicare Advantage, Medicaid (both fee-for-service and managed care), Children’s Health Insurance Programs (both fee-for-service and managed care) included.
“Payers must share data as requested by the patient by using HL7/FHIR standard securely.”
- HL7/FHIR is the future of healthcare data exchange, and it is a fundamental move away from a document-centric approach to a data-level access approach using application programming interfaces or API.
- health3D.ai supports canonical standards such as FHIR, HL7 out of the box and can be interfaced with all REST compliant services.
- health3D.ai has support for 275 FHIR resources and is customizable to accept on demand basis resources.
Risk Scoring and Stratification Methodology
Patient Segmentation
Unique Priorities, Different Needs
Enables health plans & providers to identify the right level of care and services for distinct subgroups of patient.
Segmenting the population according to health care needs allows health centers to do a better job of targeting resources more efficiently and at a lower cost.
Using traditional and modern methodologies, health3D.ai classifies members into
- Highly complex
- High-risk
- Rising-risk
- Low-risk
Risk Stratification assigns a risk status to patients, then uses this information to direct care and improve overall health outcomes. Risk Stratification prioritizes patients into distinct groups of similar complexity and care needs.
A Deep Learning Model for Member Risk Stratification
Tensorflow & Keras Based Deep Learning
Proven Methods Outperform Individual Practioners
Traditional models for patient risk prediction rely on practitioner expertise and domain knowledge. Deep learning models have proven to outperform the traditional risk models in prospective hospitalization prediction.
health3D.ai built with Tensorflow & Keras based deep learning trained models for advanced risk stratification. health3D.ai utilizes complex clinical and financial data for population risk stratification, some but not limited to member’s longitudinal health records including diagnosis, demographic, financial, and provider data.
AI Services
Reduce Human Error
Identify Care Gaps and Adapt to Change
AI is the fabric on which the healthlligence platform is built on. Most components are modeled to use continuous training and prediction services in health3D.ai. Using industry knowledge and vast amounts of data we have trained our machine learning algorithms to specifically automate care manager’s routine tasks to enhance productivity and reduce the number of errors and increase patient satisfaction.
health3D.ai recommends care plans, identifies care gaps, alerts based on an anomaly in a member’s quality measures. It acts as a virtual nurse by interacting with patients via healthwallet.me by providing education material based on condition.
health3D.ai continuously learns from Care managers and patients and adopts to change in business rules. Similarly health3D.ai can be extended for other tasks or use cases.
Anomaly Detection models to identify abnormal patterns in Member’s observations
Detect Deviations in Patient Health
Cross Reference Past, Present and Ongoing Conditions
Our approach aims to identify patient management actions for a given patient that are highly unusual with respect to past patients with condition(s) that are similar to the ones that the given patient suffers from. Once a deviation is detected, it may be used to generate a member-specific alert for consideration by the clinician(s) who are caring for the patient. health3D utilizes techniques like contextual anomalies in time-series data and collection anomalies based on defined period of Member’s vitals to detect anomalies and will report it for action.
Machine Learning models to infer business rules from historic data
Predicting Outcomes
Historical and Future Data Cycles
health3D.ai ML algorithms train from historical data (the values associated with specific input features/variables) and then apply that learning on new data in the form of predicting an outcome—and then cycle through that process iteratively. Below are a few significant algorithms that are built to help our customers.
- Identifying Disease progression
- Fall detection Risk
- Behavioral health disorders: Predict whether a member will have a diagnosed behavioral health condition, specifically depression, based on a set of input variables
- Readmission Risk
- Social networking posts analysis to detect Temporal Patterns of Help-Seeking behavior on mental health problems
